Fibroids 101

You are not alone - By age 50, nearly two-thirds of women experience uterine fibroids.¹
What are fibroids?
Uterine fibroids are non-cancerous growths of the uterus or womb. They are also called fibroids, uterine leiomyomas or myomas.²
They can be undetectable, or the size of different fruits (Ex: from a grape to a melon). Fibroids can push up against other organs and/or become a heavy mass in the abdomen sometimes reaching as high as the rib cage.
Approximately 26 million women in the US have been diagnosed and are currently living with uterine fibroids. However, there remains a significant number of women that are undiagnosed and potentially coping with the symptoms unaware of this potential condition.³
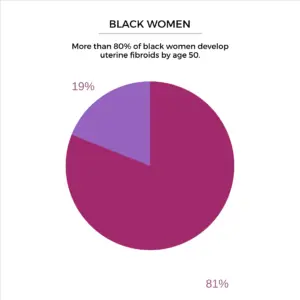
According to a 2013 US study of 1,364 women aged 35–49, more than 80% of African-American women and nearly 70% of Caucasian women develop uterine fibroids by age 50.⁴
Signs and Symptoms

If you have fibroids, you may or may not experience symptoms. Many women are not aware they have fibroids until a provider finds them in a routine physical exam or are randomly found on an imaging test (hyperlink to diagnostic tests). Other women experience significant discomfort or pain as a result of their fibroids. Everyone is different.
Some common symptoms may include:
- Heavy Menstrual Bleeding (HMB)
- Blood Clots
- Anemia
- Abdominal Cramping
- Pelvic Pain
- Back Pain
- Leg Pain
- Bulk Symptoms
- Pain with sexual intercourse (known as dyspareunia)
Heavy Menstrual Bleeding (HMB)
The most common bleeding symptom associated with fibroids is heavy menstrual bleeding (HMB). HMB is usually defined as an excessive amount of blood flow during your period. Defining what “excessive” means is difficult because women have different perceptions of a heavy flow. However, HMB could be but is not limited to:
- Bleeding that soaks through one or more pads/tampons every hour for
several hours in a row - Needing to wear more than one pad/tampon at once to control blood
flow - Waking up to change pads/tampons during the night
- Consistently lasts more than 7 days; or
- Soils your clothes and seats.
Blood Clots
Another common bleeding symptom is passing blood clots during your period.
Anemia
Anemia, which is not a symptom but may be a consequence of HMB, is a condition where there are not enough red blood cells to carry oxygen to the rest of the body. Anemia is monitored by checking your hemoglobin level. Hemoglobin is a protein in your red blood cells that carries oxygen to your body’s organs and tissues and transports carbon dioxide from your organs and tissues back to your lungs. Therefore, if your hemoglobin is below 11-12, you are considered anemic.⁵
Fibroids can cause dangerously low hemoglobin levels because of the excessive loss of blood. The most common symptom of anemia is fatigue, which may be more severe depending on how severe the anemia is. For more information about heavy menstrual bleeding and anemia, click here.
Bulk Symptoms
Bulk symptoms can occur when fibroids grow large enough to enlarge or distort the uterus, generating pressure or discomfort in the abdomen and lower back, abdominal bloating, urinary frequency or urgency and constipation. You may also notice a protruding abdomen/belly, which could make one look like they are pregnant.⁶
Have you cancelled activities due to fibroid symptoms?
Fibroids can affect your quality of life.
Uterine fibroids can negatively impact different aspects of a woman’s life such as work, school, social activities, family and personal relationships, fertility, self-image, and physical and emotional well-being among others. Your biological racial, and socio-cultural factors can all impact how you can experience fibroids. These can exacerbate existing health disparities in terms of symptoms, diagnosis and treatment.
A US survey conducted in 2012 with women aged 29-59 years (268 African-American and 573 Caucasian women) found that African-American women were more likely to experience severe or very severe symptoms which included heavy or prolonged periods and anemia. It also found that fibroids were more likely to interfere with physical activities and missing days from work.
This research indicates that African-American women’s overall quality of life is significantly more impacted by the physical symptoms associated with fibroids than Caucasian women. The experience of painful periods for African-American women should not be downplayed and they should seek medical advice to help identify any underlying issues.
Remember that different biological, racial and socio-cultural factors may place you at higher risk or impact whether you have symptoms or not. In order to diagnose and ultimately treat fibroids it is important to understand your body, seek information and engage in informed conversations with your health professional.
References
1. Understanding racial disparities for women with uterine fibroids – Erica Marsh, M.D., M.S.C.I
2. Stewart E. Uterine leiomyomas (fibroids): Epidemiology, clinical features, diagnosis, and natural history. UpToDate.com
3. https://www.ncbi.nlm.nih.gov/books/NBK537747/
4. Marsh E et al. JOURNAL OF WOMEN’S HEALTH Volume 22, Number 10, 2013
5. https://www.mayoclinic.org/diseases-conditions/ uterine-fibroids/diagnosis-treatment/ drc-20354294
6. Stewart E. https://www.uptodate.com/contents/uterinefibroids-beyond-the-basics
You are not alone
By age 50, nearly two-thirds of women experience uterine fibroids¹
Join Our Community